Cutting Investment into D+I Leadership Does Not Serve the NHS
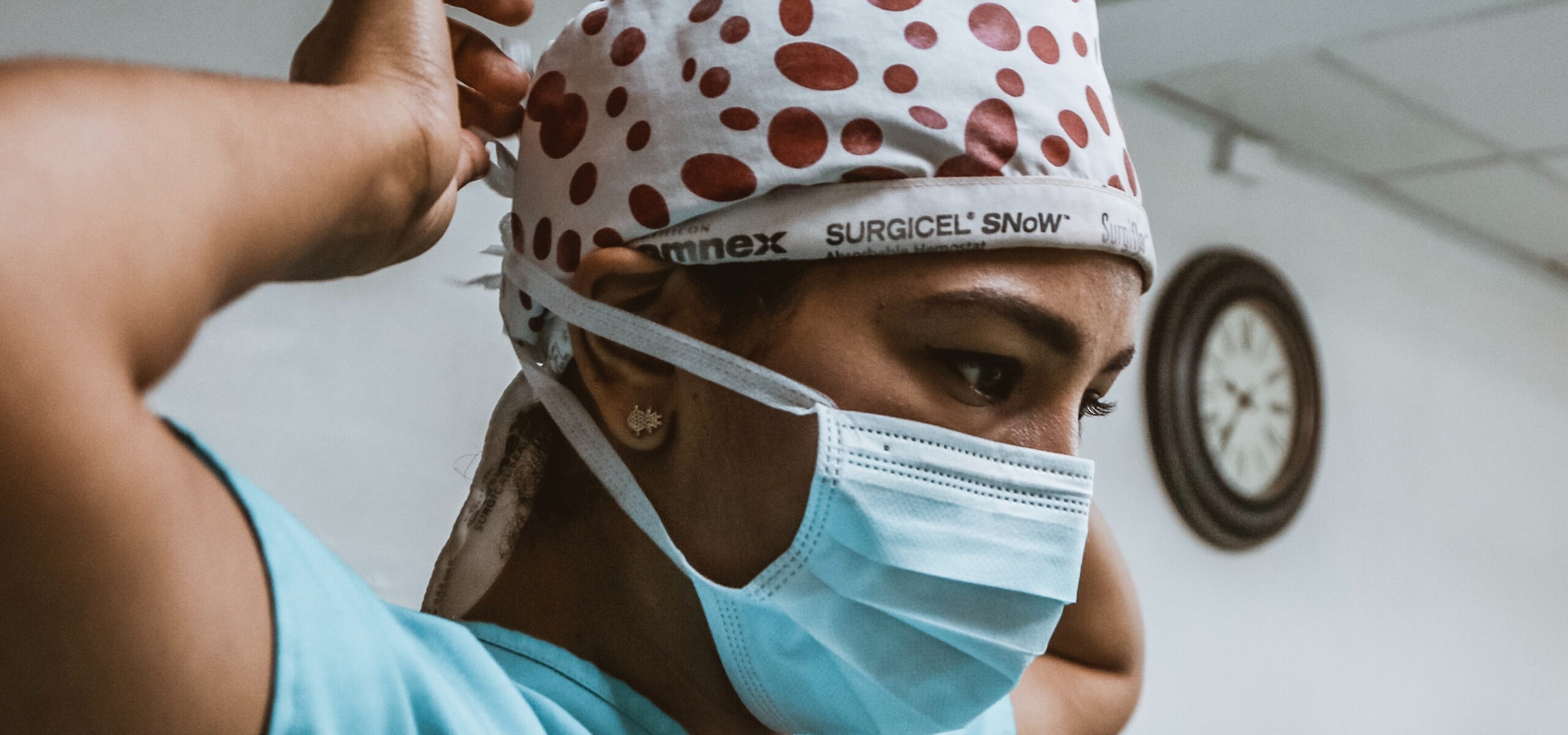
It is not news to anyone that the NHS has had to make many tough spending decisions. It has experienced over a decade of underfunding since 2010, and recent rising energy costs and inflation are more generally reducing the value of the budget it is assigned. Though it hasn’t received as much news coverage as one might expect from something so consequential, investment into Diversity and Inclusion (D+I) leadership is the latest in the long line of dominos to fall down.
It was recently reported that the NHS has significantly reduced leadership targets on D+I and D+I-dedicated teams, as Health Secretary Steve Barclay stated his intention to ‘reduce NHS micromanagement’ due to NHS bosses spending millions on ‘woke non-jobs’. As a result, NHS trusts will no longer be required to improve racial disparity among senior management and numerous staffing standards have been removed from the 2023/24 guidance, including to ‘continue to support the health and wellbeing of our staff…through effective health and wellbeing conversations’.
The issue has been largely framed as a binary ‘either-or’ decision: to allocate funding to D+I or to patient care. And this may seem hard to argue when we know that the NHS is in dire straits: critical care patients are being treated in hospital corridors and one nurse recently and devastatingly claimed that ‘it’s a good day when nobody dies in the waiting room’. But whether to spend on D+I or patient care misses the point; There isn’t a zero sum trade off between the two and the truth is that you cannot have good patient care without racial equality.
Only last year, the Health and Social Care Review (which consisted of over 1,000 interviews with front-line staff, managers and leaders in health and social care across the UK) found ‘evidence of poor behaviours and attitudes such as discrimination, bullying and blame cultures in certain parts of the health and social care system, with some staff in the NHS in particular not feeling comfortable to speak up.’
Another report by the British Medical Association reported that a staggering 42% of Black and 41% of Asian doctors have considered leaving or have left their jobs in the past two years due to racism from colleagues and patients. One junior doctor even testified to being called a ‘headscarf b**ch’ by a patient, with another refusing to be seen by her as her name ‘didn’t sound British’. All the while her supervisor did not want to discuss the experience – meeting her with silence instead.
How can medical staff be expected to perform at their best within this sort of toxic environment? How can they focus on patient care when nobody is focusing on theirs?
And it’s not just the staff who suffer either. Not only do two thirds of Black Britons believe the NHS ‘does less to protect their health than that of white people’, but data released in 2021 actually found Black women in the UK to be four times more likely to die in pregnancy and childbirth.
How is sidelining racial equality in the NHS investing in these patients’ care? The government’s framing of the issue as a matter of prioritising D+I or patient care reveals that they are only really interested in prioritising one type of patient’s care. When the system discriminates at its core, only one specific type of patient is understood as the ‘average’, and only certain types of employees can rise to the surface.
The reality is that if D+I was interpreted by the Health Secretary as a waste of money, then it wasn’t implemented effectively. What matters is not so much having one dedicated team that ends up isolated and ignored, but having an embedded set of goals and values that run through all leaders’ respective areas. It’s about entrenching de-biasing processes, accountability and active empathy. Our report from 2020, Rewiring Meritocracy, outlined five principles for achieving this sort of inclusive leadership, which the NHS should be focusing on implementing into its systems of management – at the very least.
Contrary to what the government might think, D+I within the NHS is not tokenistic “wokery” but a political imperative with very real implications for staff and patient wellbeing, and it must be treated accordingly.

